Exploring sex and gender differences in the Alzheimer’s disease patient journey: A survey study
10 September, 2025
Alzheimer’s disease (AD) affects millions worldwide, and women account for nearly two-thirds of all cases. Yet little is known about the different experiences of men and women affected by the disease. A new study, published by the Women’s Brain Foundation (WBF) in collaboration with Charles River Associates (CRA), sheds light on the differences between men and women in the AD patient journey – from awareness and diagnosis to treatment and quality of life. These insights are critical for advancing prevention, improving diagnostic accuracy, and ensuring more equitable care.
The research was based on a structured survey of 142 participants—both patients and caregivers—in
the United States and Germany. The results provide important evidence to guide precision medicine approaches in AD.
Key Findings
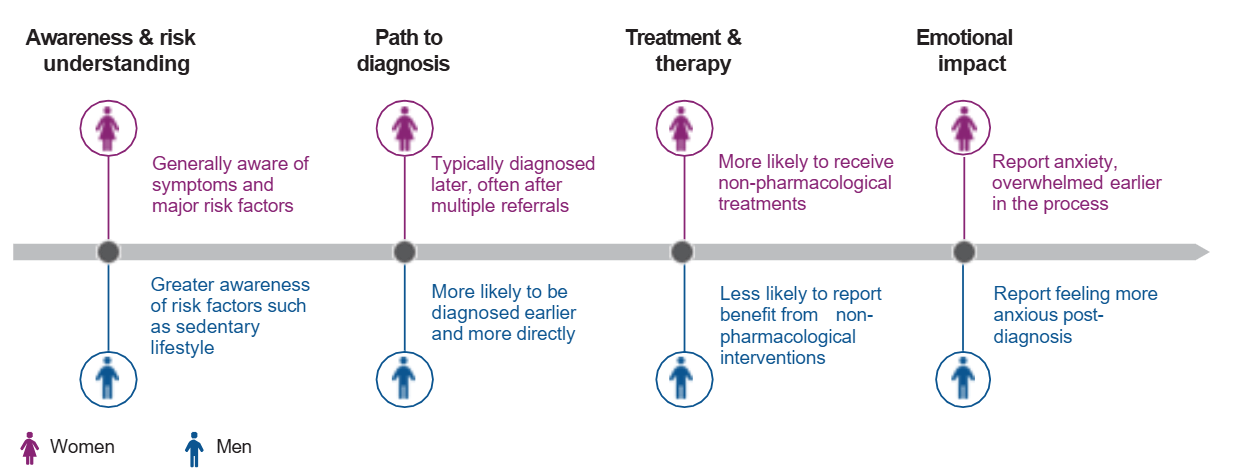
– Awareness of risk factors
Both men and women were familiar with the disease and demonstrated similar levels of awareness regarding major risk factors for AD, such as old age, genetics, hypertension, and loneliness. However, men reported increased awareness of lifestyle-related risks compared to women, particularly regarding sedentary behavior. This knowledge gap is concerning since regular physical activity reduces the risk of AD. Targeted educational campaigns are needed to promote prevention strategies equally among women and men.
– Pathways to diagnosis
Women were more likely to receive a diagnosis only after referral to a specialist, while men were often diagnosed by the first doctor they consulted. Importantly, the study showed that diagnosis was faster when a specialist was involved, regardless of sex or gender—underscoring the value of timely access to neurologists and memory clinics.
– Symptoms prompting diagnosis
Women more often sought medical advice due to forgetting recent conversations or events. This suggests that certain memory symptoms may be more noticeable for women or their caregivers, potentially leading to earlier healthcare-seeking behavior.
– Treatment approaches
Women were more frequently treated with non-pharmacological therapies such as reminiscence therapy or life story work, which are known to improve emotional well-being. Identifying such differences in treatment preferences can help healthcare providers tailor therapies to each patient’s needs.
– Emotional Journey
Women reported higher levels of anxiety at the beginning of the diagnostic process, whereas men expressed greater distress after receiving a formal diagnosis. Recognizing these emotional patterns can guide healthcare professionals in providing more personalized psychological support.
Why it matters
This study highlights the importance of integrating sex and gender perspectives into every stage of the AD patient journey. From awareness to treatment, men and women face different challenges that shape their experiences and outcomes. Addressing these differences could lead to:
- Earlier access to specialists
- More accurate and timely diagnoses—especially for women
- Tailored treatment options that align with patient preferences
- Better emotional support for both patients and caregivers
By embedding sex and gender considerations into research, healthcare, and policy, we can move toward more precise and equitable care for all people affected by Alzheimer’s disease.
Read the full study here